Impact of a Crisis on Waste Management Policy Adherence And Practices - A Narrative Review of Bio-Medical Waste Management During the Covid-19 Pandemic
1
School of Engineering and Technology,
National Forensic Sciences University,
Gandhinagar,
Gujarat
India
2
Department of Environmental Science,
National Forensic Sciences University,
Gandhinagar,
Gujarat
India
3
, Loyola Centre for Research and Development,
St. Xavier's College Campus,
Ahmedabad,
Gujarat
India
4
Department of Environmental Science,
Gujarat University,
Ahmedabad,
Gujarat
India
Corresponding author Email: jondcosta63@gmail.com
DOI: http://dx.doi.org/10.12944/CWE.18.3.05
Copy the following to cite this article:
Costa J. D, Patel H, Braganza V, Solanki H. Impact of a Crisis on Waste Management Policy Adherence And Practices - A Narrative Review of Bio-Medical Waste Management During the Covid-19 Pandemic. Curr World Environ 2023;18(3). DOI:http://dx.doi.org/10.12944/CWE.18.3.05
Copy the following to cite this URL:
Costa J. D, Patel H, Braganza V, Solanki H. Impact of a Crisis on Waste Management Policy Adherence And Practices - A Narrative Review of Bio-Medical Waste Management During the Covid-19 Pandemic. Curr World Environ 2023;18(3).
Download article (pdf) Citation Manager Publish History
Select type of program for download
| Endnote EndNote format (Mac & Win) | |
| Reference Manager Ris format (Win only) | |
| Procite Ris format (Win only) | |
| Medlars Format | |
| RefWorks Format RefWorks format (Mac & Win) | |
| BibTex Format BibTex format (Mac & Win) |
Article Publishing History
| Received: | 2023-06-14 |
|---|---|
| Accepted: | 2023-08-04 |
| Reviewed by: | 
 Faheem Ahamad
Faheem Ahamad
|
| Second Review by: |

 Rishikesh Singh
Rishikesh Singh
|
| Final Approval by: | Dr R K Aggarwal |
Introduction
Health experts have linked uncommon occurrences of pneumonia that occurred in Wuhan, a city in China, in December 2019 to the wet market, a place where live animals are sold for consumption 1. The precise pathway to human infections is still unknown as a result of the lack of initial emphasis given to research to find intermediate hosts 2,3. Ophthalmologist Dr. Lee Wein attempted to alert medical professionals about this virus by describing its symptoms. At the age of 34, he passed away from this infection in February 2020. Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV2), aka COVID-19, first gained global recognition in January 2020 as a result of the World Health Organization's (WHO) reporting of these cases4. WHO's Research and Development department implemented diagnostic and therapeutic approaches that employed reverse polymerase chain reactions for diagnosis and the sequencing of genomes for initial laboratory evaluations because of the escalating infections in China and the other regions 4 of the world 5. As a result, a global emergency was proclaimed in January 2020. The coronavirus family — with Covid-19 being a prominent part of it, can infect both people and animals 6.
The first researchers on this category of viruses were Bynoe and Tyrell in 1966. They studied them by isolating them from people who had the common cold and named them coronaviruses because of their structural resemblance to a solar corona. Global pandemic COVID-19 has caused a number of logistical and environmental problems, most notably in the form of BMW. In February 2020, Wuhan, the COVID-19 centre, generated more than 200 tonnes of biomedical waste, that's four times the amount of waste that could have been stored in the city. As a result, it was assumed that clinical waste and the number of confirmed cases are connected. Waste management companies worldwide are taking the necessary steps to guarantee that healthcare facilities treating individuals with Covid have been disinfected 7. The study seeks to highlight how this global epidemic has affected the current systems for handling waste.
Bmw Management Before and After the Pandemic - Case of India
In India, there are only 198 Common Biomedical Waste Treatment Facilities (CBMWF) and 225 captive incinerators that can manage the 2,00,000 tonnes of BMW that accumulate there every year. By 2022, India is expected to produce 775.5 tonnes of BMW per day, a significant increase from the present 550 tonnes per day (Assocham-Velocity MR study, 2018). BMW was expected to increase at a CAGR of about 7%, as per the report. According to socioeconomic and demographic characteristics, not everyone is being impacted equally by COVID-198. It is difficult to fully comprehend why infectious behaviors affect various socioeconomic strata in distinct manners, with accuracy of data being the main concern. Important socioeconomic characteristics are crucial since, regrettably, Covid - 19 has a substantial influence on underdeveloped areas 9. Education, rural or metropolitan setting, demography, and the overall number of tenants per residence are some of these indicators.
About 619 tonnes of BMW were generated in India on a daily basis, just before the pandemic 10. Over 47% of the BMW generated in India before the pandemic can be attributed to five states, namely Kerala, Uttar Pradesh, Tamil Nadu, Maharashtra, and Karnataka, the latter being the largest contributor of the same. The highest single-state BMW generation rate was equal to 77.5 tonnes per day, or 77,500 kgs. During the pandemic, the drastic increase in the usage of PPE kits and other medical gear led to a sharp rise in the BMW generated. Consider that during the height of the pandemic in India, nearly 2.5 million PPE kits were needed each day to prevent the dissemination of the virus to get an understanding of the sheer magnitude of this rise. Estimates show that in one state, Kerala, which also had the highest ranking in terms of C-BMW (Covid-Biomedical Waste) output throughout the second surge of virus, approximately 250,000 kgs of BMW were produced just with pandemic-based measures like PPEs per day. It should be recognised that this is in addition to the typical BMW production rates that were common prior to the outburst of the epidemic. In essence, the usual generation of biomedical debris associated with COVID alone during the pandemic in India reached 203 tonnes per day 11. It is in the light of such facts that the question becomes pertinent as to how this massive increase in BMW waste generation impacted policies and processes associated with the management of such forms of waste. The aim of the study is to understand, via the route of a narrative review of studies conducted on the subject in the aftermath of the pandemic, as to how the existing infrastructure and policy frameworks held up in the face of what can be aptly called a major waste management crisis.
COVID-19, the global crisis, had a number substantial effects, including a significant upsurge in the production of biomedical debris relative to levels and rates that were usual in the years before the outbreak 12. The substantial increase in BMW during the pandemic coupled with the pressure that the crisis placed on existing systems and practices of management, were crucial factors in shaping the way the issue of waste management was dealt with in India and abroad. The study at hand explores how the pandemic impacted BMW management practices and policies over the course of the major lockdowns that were levied during 2020 - 2022. The objective of the study is to identify the changes, if any, in practices and policies that were brought forth as a result of the pandemic, and to recognize the reason behind these changes and shifts in order to understand how to prepare for the next looming crisis.
Bmw Components and the Threat They Pose
Any waste generated during the creation or testing of biological products, as well as the waste categories described in Schedule 1, are considered to be biomedical waste. Additionally, it includes waste created when humans or animals undergo examinations, treatments, or immunization. Any garbage that has infectious or possibly contagious elements is included. This term covers garbage produced by healthcare facilities such as clinics, hospitals, dentistry offices, labs, and facilities for doing medical research. Blood and other biological fluids, as well as other pollutants, can be found in biomedical waste. The Medical Waste Tracking Act of 1988 delineates medical debris as any refuse produced during the process of examining, studying, appraising, inoculating, or providing medical care to humans or animals. According to the Gazette of India, GSR. 343(E), published on March 28, 2016, BMW can encompass a wide range of various healthcare industry byproducts. It employs the "cradle to grave" methodology, characterising, quantifying, classifying, storing, transporting, and treating BMW. The most typical waste categories, as determined by recent studies, are shown in the table below 13.
Table I: Common Waste Categories 13
| SR NO | WASTE CATEGORY | DESCRIPTION |
| 1. | SHARPS | Objects that can pierce the skin are included in this type of waste, including syringes, surgical knives, pricking tools, broken glass, shaving blades, tiny sealed containers, clamps, filaments, and sharp surgical equipment. |
| 2. | Infectious Waste | Any substances carrying infections or the potential for infection, including connective tissue, lab cultures, equipment, and wipes. |
| 3. | Radioactive Wastes | This category of debris typically refers to surplus radiotherapy fluids that haven't been utilized, or liquids employed in laboratory experiments. |
| 4. | Pathological | Flesh, tissue, organs, and bodily fluids of humans. |
| 5. | Pharmaceuticals | This category encompasses any vaccines and medications that are not used, have expired, or have become tainted. |
| 6. | Genotoxic Waste | This constitutes an extremely perilous type of BMW, possessing properties that can lead to cancer, birth defects, or genetic alterations. Furthermore, it may encompass cytotoxic medications. |
| 7. | General non-regulated Medical Waste | Referred to as non-risk waste, this category lacks any specific chemical or biological threat. |
According to the paper stated above, biomedical wastes (BMW) are potentially hazardous waste products which comprise laboratory waste, solid and liquid components, and sharp objects/items, all of which are slated to pose a major risk to both humans and other living things. It may also be fatal in some circumstances. Therefore, it is crucial that this waste be properly managed and disposed of in order to stop an infectious outbreak that could harm humanity. Furthermore, it must not disturb the health care settings in society. For example, during this past COVID situation, they found a heavy amount of waste generated by the hospital and laboratories, which poses a threat to new diseases if the waste is not handled correctly. Therefore, theyinsist that appropriate care and precautions are a must while disposing of the biomedical waste not to infect the population.
Regarding BMW, handling involves the generation, categorization, separation, gathering, storage, wrapping, loading, conveyance, and unloading of such refuse, along with their handling, management, elimination, conversion, and trade, transfer, or removal.
Main Sources of Biomedical Waste
Since the outbreak of the novel coronavirus, Ilyas et al. studied home quarantine, institutional quarantine and isolation wards and facilities, and found that these were generating significant amounts ofBMWglobally 14. Testing kits, surgical face masks, nitrile gloves, and personal protective equipment (masks, gloves, gown/overall, shoes, caps, goggles, eyeshields, etc.) are the main sources of trash. The incineration of an entirely novel BMW type (COVID waste), if not treated properly, poses a significant risk to the global sustainability of the environment and human health. Garbage might lead to the exponential spread of SARS-CoV-2, a lethal virus that could stay around for a maximum of seven days on covid trash (such as face masks).
In contrast to copper or cardboard, the stability of the virus was greater on plastic and steel, as indicated by a scientific study examining aerosols and the durability of surfaces 15. Hence, this compels us to implement efficient COVID waste disposal systems, to reduce the possibility of pandemic transmission and to manage environmental threats sustainably 16. The numerous technologies for treating COVID-waste have been evaluated in the sections that follow, from its distinct collection to a range of chemical and physical processing steps. The use of various disinfection approaches has also been considered in policy briefs on the international campaigns for managing COVID-waste, with certain possible applications successfully used to reduce health and environmental problems.
Figure 1 below presents the segregation of BMW into various segments:
- Using separate colour-coded bins
- Using double layered collection bags.
- Appropriate labelling of the bins.
- Handling by authorised and trained staff.
- Stored in a separate storage room.
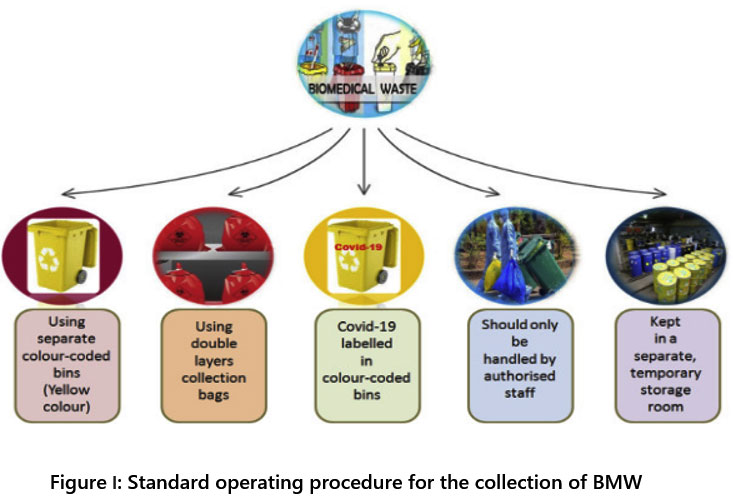 | Figure I: Standard operating procedure for the collection of BMW
|
Source:- Shobhana Ramteke, Bharat Lal Sahu, Novel coronavirus disease 2019 (COVID-19) pandemic: Considerations for the biomedical waste sector in India, Case Studies in Chemical and Environmental Engineering, Volume 2, 2020, 100029]
The above diagram shows the various bags and various methods used to collect biomedical waste from laboratories and hospitals. These methods can be more useful and effective as safety measures. Due to these proper collections and disposal methods, we can easily prevent or reduce the risk for the COVID-19.
Narrative Review of Core Studies
Clash between CPCB Policies and Other Government Frameworks
A review of different strategies used to dispose of biomedical waste (BMW) during a pandemic reveals that many hospitals complied with the guidelines for doing so, including the advice to use double-layered packs (using two bags), the directive to label bags and holders as "COVID-19 waste," the regular sterilisation of designated carts, and the segregation of garbage generated by COVID-19 isolation chambers into distinct records. Even though the CPCB is the official organisation for releasing any recommendations regarding BMW in the Indian subcontinent, other government authorities have also published specific guidelines to address COVID-19 waste.The 2016 BMW Management Rules, which are based on the ultimate method of medication, have various changes in how the products are divided up, even if the latter policies must follow the CPCB's guidelines. For certain BMWs, the unexpected shift in categorization could result in improper last treatment. Their proposals to incorporate a particular URL for the CPCB policies and to clearly state in various governmental entities' regulations that the criteria set by the CPCB shall be adhered to in the case of BMW are extremely essential. Along with preserving uniformity, BMW management should give the following priority when monitoring the application of the recommended policies.
Due to the rise in the volume of this trash, hospitals and other institutions need to strengthen their ability to transport and store BMWs
The precise amount of "COVID-19 waste" in each category should be communicated electronically
Any breach that occurs while being transported or treated needs to be reported to the nodal agency
The organization's prevention and control of infections department should regularly train all affected staff members and should monitor the protocols.
These actions will assure a more effective handling of the forthcoming crisis, together with rigorous respect to the rules.
The Policy Framework Evolution During COVID-19 Pandemic
Biomedical trash generated sky-rocketed predominantly after the SARS Cov2 commencement. BMW being highly infectious and contaminated, which poses a massive challenge to all the stakeholders involved in its management to avoid spreading COVID-19 through it. Researchers have emphasised the need to monitor the complete cycle, from the cradle to the grave, if the spreading conditions are controlled 17. For all parties involved, including laboratories, urban local bodies, isolation centres, quarantine facilities, sampling centres, and the Common Bio-medical Waste Treatment Facility (CBWTF), he continued, the production, acquisition, preservation, transportation, and elimination of Covid-19 debris is a significant challenge. The Indian authorities have autonomously formulated the Directives for Managing COVID-19 Medical Waste, which should be adhered to alongside the Biomedical Regulations of 2016, with the aim of constraining the transmission of the coronavirus via this means. This is because it is a unique virus. A suitable Covid waste management system was implemented to prevent the virus' transmission in India due to its unusual origin and the absence of comprehensive information about its behaviour, even though no formal instructions were provided until mid-March 2020. It was imperative because, before the pandemic, only 265 tonnes per day were undergoing treatment. The Epidemic Disease Act of 1897 was passed as the first significant step, allowing the Central Government of India to issue direct orders to the State Governments. On March 18, 2020, the Central Pollution Control Board (CPCB), a segment within the Ministry of Environment, Forestry, and Climate Alteration of the nation, issued comprehensive guidelines (CPCB 2020a, 2020b, 2020c, Guidelines for handling, treatment, and disposal of waste generated during treatment/diagnosis/quarantine of Covid patients, https://cpcb.nic.in).
The Directives concerning the virus, BWM, were notified in March 2020, and after that, a second revision was made on 19th April 2020. They set forth seven key criteria for all parties involved in the appropriate collection, handling, and removal of medical debris associated with COVID-19-infected patients, including healthcare facilities (HCF), isolation centres and residences, obtaining samples centres, labs, ULBs, PCCs, SPCBs, and CBWTFs.
Process-level Issues in BMW Management during the Pandemic
Biomedical waste management is both a socially significant obligation and a regulatory need. In order to do this, studies have examined the real-world difficulties associated with handling and removing biomedical debris in a few hospitals in Ahmedabad 18. A total of several categories of biological wastes produced over the course of four months were examined. They correctly assert that employees in the healthcare industry must be aware of the risks posed by biomedical waste in the workplace and implement scientifically sound disposal methods. The treatment and elimination of biomedical debris has been plagued by practical issues in a few hospitals in Ahmedabad. The healthcare sector is one of the top sectors in India in terms of both employment and income. Hospitals, medicinal gadgets, clinical trials, outsourcing, telemedicine, and medical care make up healthcare. The rapid growth of the healthcare sector has contributed alarmingly towards the menace of biomedical waste, which needs to be tackled sensibly and sustainably. Consequently, the Environment (Preservation) Act of 1986 was called upon, leading to the Department of the Forests, Environment, & Climate Change Division of the Ministry issuing the Biomedical Waste (Regulation and Control) Guidelines, 1998 [19]. These preceding statutes were subsequently superseded by the BMW (Administration) Guidelines of 2016. According to the new regulations, whoever handles biomedical debris must obtain authorization from the State Pollution Control Board, regardless of how much there is. The term "occupier" refers to a person who has operational control over a facility that produces biomedical debris, as defined by the current legislation. Regardless of the medical theories they use, this includes a variety of organisations including clinics, hospitals, veterinarian centres, labs, blood donation centres, and healthcare divisions. The occupier has a responsibility to take all necessary actions to ensure that such garbage is disposed of in a way that protects the environment and community health 20. Ironically, organisations dedicated to helping the sick and promoting community health unknowingly play a substantial role in disease transmission. The cost of implementing current technology for garbage disposal and the management's profit-driven behavior are the main determining factors, which force them to choose "end of the pipe" options that are simpler and less expensive, such as incineration of waste by burning it in open spaces.
The three R's—reduce, reuse, and recycle—should serve as the cornerstones of any sound BMW practice. Even better would be to avoid producing garbage altogether or to recycle as much as you can as opposed to throwing it out. In order to avoid waste, minimise it, use it again, recycle it, recover it, treat it, and then dispose of it. Therefore, rather than using an end-of-pipe strategy, waste should be addressed from the source. The following results have been reached by Deva et al. following their analysis of the total and average amounts of BMW produced by hospitals and their collection, segregation, pretreatment, transportation, and record-keeping practices11;
Multi-specialty hospitals with state-of-the-art infrastructure generate maximum waste.
These hospitals are in densely populated areas of the city.
Segregation of waste at source is not done correctly, primarily due to adhocism, fresh and untrained staff for the job temporarily. This leads to additional burden on operators at the CBWTF.
Some of the strategies recommended by them were:
Healthcare facilities should teach and raise awareness about the importance of proper BWM amongst their staff.
The facility should ensure a waste management plan and allot budget and personnel to implement the same.
Segregation of BMW should be done by trained staff only.
Transportation of the BMW through dedicated vehicles only.
Training of the staff dealing with BMW should be conducted in the language/medium they understand. In addition, regular refresher courses should be planned.
 | Figure 2: COVID bio-medical waste management personnel with a bin
|
Impact of Violation of BMW Management Rules throughout the Pandemic
The COVID-19 outbreak was researched by Kumar et al.21. The goal of this study is to give information about COVID-19 prevention, environmental concerns, social and economic effects, and medications. The best defense against COVID-19 is social seclusion, screening, lockdown, mask wear, and sanitizer or soap at frequent intervals. The ecosystem is at risk from the spread of Covid-19 through fecal-oral roots. Human garbage and medical/biomedical debris should be disposed of properly to protect the environment. Although COVID-19 has had an impact on social and economic life, there was no cure prior to the development of medicine. An integrated strategy between modern and traditional medical systems may provide an early stoppage of additional viral spread from the perspective of medicine or COVID-19 treatment. A list of herbs and medications from the Indian Medical System has been looked up and reported on based on the symptoms of COVID-19. For the purpose of developing a potential COVID-19 medication, extensive testing and clinical trials will be conducted.
It is established that due to the disequilibrium of the earth's natural system, many animals, birds, and humans are affected, and the whole ecological system of the earth is affected 22. Considering COVID-19, a naturally occurring and transmitted disease, throwing out biomedical wastes like the surgical mask, gloves, etc. in the middle of the road will affect animals, especially the cow and dogs. It can be a cause of death to the animals. Thus, with these various types of transmission, COVID-19 can find a new host 23.
Shift in Global Waste Management Dynamics during the Pandemic
The outbreak of the virus has altered the dynamics of generated trash around the world, according to a study by Sharma et al 24. This necessitates extra caution. Policymakers must also react quickly to unanticipated changes in waste mix and volume. This analysis focuses on the difficulties the epidemic is posing for the solid waste management industry as well as the possibilities that exist to close current discrepancies in the system's functioning. A specific scenario emphasized in the document involves the management of medical refuse, synthetic waste, and food remains, all of which have been notable sources of concern throughout this critical period. Lacking robust involvement and cooperation from the community, merging virus-laden medical waste with the standard solid waste flow presents grave health and safety hazards for sanitation workers. An increase in the adoption of disposable plastic is anticipated due to escalating concerns related to cleanliness, particularly in relation to personal well-being and healthcare provisions. Owing to increased recognition of the significance of accumulating durable items amid a lockdown and concerns regarding food shortages, a reduction in the generation of food waste at home is expected. Nonetheless, there exists a possibility that disrupted distribution networks may lead to the wastage of food to an increased level. Some scenarios include food provisions becoming stranded on routes due to limitations on vehicle movement, or a deficit of labor in storage facilities to manage the provisions. The analysis highlights the crucial nature of developing resilient distribution networks suited to local contexts, enabling effective response to similar situations in the event of future pandemics. While providing creative answers to the problems with waste management that are already present, the study also makes some crucial suggestions to the policymakers to assist in handling any potential pandemics that may arise in the future holistically.
The issue of how to handle the garbage problem has grown and ought to be a subject of anxiety because this waste has a high potential for spreading sickness to those nearby. During the isolation of COVID-19 patients and in the course of community examination protocols, unlabelled hazardous waste originating in places where the presence of asymptomatic carriers and infected individuals is uncertain might be managed by waste handlers, sanitation staff, scavengers, and even ordinary citizens. Expressing apprehension is crucial regarding the absence of a system and knowledge concerning the collection and disposal of the used face-masks and medical debris created by those adhering to home isolation.
By way of example, a mound of healthcare refuse near the examination zone contained discarded facial coverings, hand coverings, attire, eyewear, and headgear. These items had not been appropriately discarded in accordance with the guidelines, which stipulated the use of yellow bags for disposal. Due to a lack of space, resources, and awareness, this did result in a potential health risk for those who weren't infected as well as for health professionals, screening teams, and waste handlers. In addition, many members of the health team were lacking the full complement of personal protective equipment (PPE) necessary to protect against infection with such high trans fat levels. The relationship between COVID-19 and the management of biomedical waste was examined by some researchers. 25. The waste is hazardous and a concern, but improper waste management might make the situation even riskier. Lockdowns have been one strategy for controlling the spread, but they do not guarantee that all COVID-19 regulations are being strictly adhered to 26. Therefore, those components of proper management that are strictly followed lead to success in the end.
The Birth of New Waste Management Perceptions due to the Pandemic
The pandemic has also imparted important safety lessons to lab professionals for the future. Nobody would have believed someone who forecast the situation in laboratories around the world 18 months ago. The COVID epidemic did, however, occur that year, and it did change how laboratory medicine is practised globally27. Dan Scungio, MT (ASCP), SLS, CQA (AQA), a certified medical technologist and laboratory safety consultant, has identified three important lessons learned by many organisations, which we can take forward. While these three safety lessons may stand out as best remembered from the pandemic year, there are certainly more.
PPE
Many organisations began to stockpile PPE, purchasing it from wherever they could. In the process, they procured it from non-regular vendors and even through the internet. Though at first, it seemed like a smart strategy, it had some unexpected repercussions. This has been one of the reasons behind the implementation of new guidelines for the management and use of PPE kits by international organizations like WHO 28.
Storage of such a colossal stock was a significant issue.
Supply from non-regular vendors led to the supply of non-OSHA(Occupational Safety and Health Administration)standards, so it could not be used, as it did not provide adequate protection for the staff, e.g., replacement gloves did not protect against chemicals, respirators did not correctly fit users, and proper fit testing could not be performed.
Many received reusable lab coats but had no laundry services in place to wash them.
Standard Precautions
The threat of the Ebola Virus has reappeared after a year of working with the coronavirus and learning how to handle samples and conduct testing in the lab. The CDC (Centre for Disease Control and Prevention) has started screening visitors to the US in order to help manage this terrible disease following a recent epidemic in Africa. The conflict between humans and the world's pathogens is not new and is not about to end. Specialists are already keeping an eye on a number of additional zoonotic infections to see if they may be the source of the upcoming pandemic of infectious diseases. The knowledge of bloodborne and airborne pathogens is a must for laboratories. However, since the lab workers are aware that their surroundings can have an impact on others' safety, this will need to be an ongoing, continual practise. The lab staff is helped to recall that they work with hazardous materials in an environment that is intrinsically unsafe every day by this continual training that is centred on pathogen safety. The lesson gained going forward is the significance of that ongoing education about pathogens and safe lab practises that will safeguard laboratorians from hazardous chemicals and pathogens, even in the presence of engineering controls, PPE, and Standard Precautions 29.
Move Quickly Ahead- but Safely
One last lesson that many laboratories took away from 2020 was the necessity of moving quickly to integrate new testing and new practises while maintaining safety. In the last few years, laboratories have spent most of their time locked away in basements. Administrators had to supply the infrastructure, resources, and other necessities to handle this increased workload at a rapid pace due to the need for COVID-19 testing. As a result, test procedures were often set up in inadequate spaces, biological safety cabinets (BSC) were insufficiently common, and adequate environments (temperature, humidity, ventilation, etc.) were not always present. In some instances, testing was also implemented so quickly that staff safety and training were not adequately addressed. These unfavourable outcomes led to the conclusion that, in order to go forward with a new process swiftly, there should be a step-by-step generic process in place, allowing vendors, facility employees, IT specialists, and everyone else involved to collaborate to bring about quality new testing.
While these are only three lessons, there are certainly more to consider. For instance, while sourcing equipment, making sure a representative from the laboratory safety is involved in the purchasing decision is crucial. This will save a great deal of time later on. The CDC has also certified that certain respirators function well past these given expiration dates. Finally, due to the PPE shortages, the CDC created new guidelines for extending and reusing specific protective equipment. For example, it was announced that some disposable lab coats could be laundered and reused.
Conclusion
Even while the pandemic resulted in a substantial death toll from infection alone, the population faces a lesser-known but very serious hazard from an inability to appropriately treat bio-medical waste in such a situation. Therefore, it was crucial to conduct a narrative review study on how COVID-19 and the handling of biomedical debris interacted in order to identify the reasons why traditional systems crumbled when confronted with novel sources and forms of BMW. The risks of COVID-19 spreading inside communities can exceed anticipated levels and cause the loss of more lives in the coming days if the enormous amount of medical waste cannot be controlled by maintaining correct and adequate rules 30.
Significant management challenges arise in the safe disposal of COVID-19 from the point of manufacture to its final treatment centres. The treatment facilities will be overwhelmed by such a volume of wastes as the cases rise exponentially. Combining conventional medical trash with biomedical waste, particularly food waste from COVID-19 wards, is also quite difficult. India must therefore carefully supervise COVID-19 waste disposal if it hopes to stop further illness outbreaks.
The only means of containment are simple methods of infection control, as is clear from the pandemic's current state. The management and disposal of waste properly is a crucial component of these control methods. This paper aims to draw attention to not only the proper management of BMW during medical crises but also to the underlying causes and forces that result in the subversion of current policy frameworks and processes that tend to function 31.
As per the narrative review conducted via this study, some of the core reasons behind the violation of BMW management policies and processes were identified, namely:
Discrepancies caused due to clashing statements between guidelines given by CPCB and other government agencies -
The lack of a cohesive policy framework across state government jurisdictions dedicated to COVID-19 based waste disposal led to a lack of clarity and the inability to adapt quickly to the rise in BMW during this time
Adhocism
The increased pressure and build-up of BMW coupled with the rising socio-cultural pressure of rising cases often resulted in the co-mingling of virus-laden waste with normal waste due to the inability of existing systems to accommodate the change seamlessly
Personnel-level issues
Untrained staff and freshly recruited individuals without experience had to be brought in to cater to the sudden rise in BMW and the need for more hands on deck to manage the surge in waste management capabilities
Inadequate information infrastructure and awareness
Lack of adequate awareness about thedisposal of masks and other COVID-related items among households, especially among quarantined individuals, resulted in the disruption of the waste management cycle right at the source
Lack of authentic sourcing
Lack of safe and authentic sourcing of PPE kits, masks and other virus management equipment due to increasing demand for the same led to several unsavoury situations and practices
- Lack of adequate storage facilities and sudden management shock due to quantity rise led to more waste generation
- Lack of authentic sourcing also led to direct increase in waste via low quality material that was unfit for usage, resulting in shorter use cycles
In essence, the study found through a holistic review of the waste management scenario during the pandemic that several factors aligned together to cause disruptions in the existing systems and policy frameworks. Even though central waste management guidelines were developed specifically for the pandemic, lack of adequate implementation of the same on a State level and the clash between government agencies and nodal agencies in terms of standardised practices led to disruption of processes. Other than this, the study also found that several socio-cultural factors, such as human labour demand increase, equipment demand rise and the resultant increase in black market trade, and other such factors also contributed to the violation of guidelines and processes 32. In conclusion, it is to be noted that on the eve of a medical crisis, governments have to consider more than merely the development of a central policy framework for BMW management, but further invest in training, awareness, and socio-cultural capability building in order to ensure that system shock is avoided and that waste management can be used as a tool for reducing infection spread rather than encouraging it. In other words, the management of bio-medical waste during a medical crisis like the COVID pandemic, demands looking beyond the immediate concerns and adopting a larger picture approach to the problem33. It is crucial for policymakers to consider socio-cultural, environmental, organisational, and economic factors in order to prepare a nation for a medical crisis from the point-of-view of waste management in particular. System shock and overburdening of processes is inevitable in a nation if policymakers are unable to consider the breadth of the waste management issue, from awareness at the point of waste generation to training, purchasing behaviour, and other factors that extend beyond immediate systematic concerns.
Acknowledgements
I would like to thank my guide Dr. Harshad Patel for helping me throughout my review article. I would like to thank Dr(Fr) Vincent Braganza for proof reading my article. I would also like to thank Dr. Priyanka Dube for helping me edit my research article.
Conflict of Interest
The authors declares no conflict of interest.
Funding Sources
There is no funding or financial source for this this research work.
References
- World Health Organization. Rational use of Personal Protective Equipment (PPE) for coronavirus Disease (COVID-19). Interim Guidance. 2020. https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nC0V-IPCPPE_use-2020.2-eng.pdf.s
- Li M, Lei P, Zeng B, Li Z, Yu P, Fan B, Wang B, Li Z, Zhou J, Hu S. Coronavirus disease (COVID-19) spectrum of CT findings and temporal progression of the disease. Acad Radiol. 2020. doi:10.1016/j.acra.2020.03.003
CrossRef - Zhou YXL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270-273. https://doi.org/1038/s41586-020-2012-7
CrossRef - Wang D, Hu C, Hu B, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069. doi:10.1001/jama.2020.1585
CrossRef - Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) outbreak: what the department of radiology should know. J Am Coll Radiol. 2020;17:447-451. doi:10.1016/j.jacr.2020.02.008
CrossRef - Luan PT, Ching CTS. A reusable mask for coronavirus disease 2019 (COVID-19). Arch Med Res. 2020;51:455-457. doi:10.1016/j.acra.2020.04.001
CrossRef - Collivignarelli MC, Abba A, Bertanza G, Pedrazzani R, Ricciardi P, Miino MC. Lockdown for Covid in Milan: what are the effects on air quality? Sci Total Environ. 2020;732:139280. doi:10.1016/j.scitotenv.2020.139280
CrossRef - Messner W. The institutional and cultural context of cross-national variation in COVID-19 outbreaks. medRxiv. 2020. https://doi.org/10.1101/2020.03.30.20047589
- CPCB. Annual report on biomedical waste management as per Biomedical Waste Management Rules, 2016 for the year 2019 (2019b). https://cpcb.nic.in/uploads/Projects/Bio-Medical-Waste/AR_BMWM_2019.pdf
- Dehal A, Vaidya AN, Kumar AR. Biomedical waste generation and management during COVID-19 pandemic in India: challenges and possible management strategies. Environ Sci Pollut Res Int. 2022;29(10):14830-14845. doi:10.1007/s11356-021-16736-8
CrossRef - Saxena P, Pradhan IP, Kumar D. Redefining bio medical waste management during COVID- 19 in india: A way forward. Mater Today Proc. 2022;60:849-858. doi:10.1016/j.matpr.2021.09.507
CrossRef - Hirani DP, Villaitramani KR, Kumbhar SJ. Biomedical Waste: An Introduction to its Management. Int J Innov Res Adv Eng. 2014;1(6)
- Ilyas S, Srivastava RR, Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci Total Environ. 2020;749:141652. doi:10.1016/j.scitotenv.2020.141652
CrossRef - Van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564-1567. doi:10.1056/NEJMc2004973
CrossRef - Bashir MF, Ma BJ, Bilal, et al. Correlation between environmental pollution indicators and COVID-19 pandemic: A brief study in Californian context. Environ Res. 2020;187:109652. doi:10.1016/j.envres.2020.109652
CrossRef - Ranjan MR, Tripathi A, Sharma G. Medical Waste Generation during COVID-19 (SARS-CoV-2) Pandemic and Its Management: An Indian Perspective. Asian Journal of Environment & Ecology. 2020;13(1):10-15. doi:10.9734/ajee/2020/v13i130171
CrossRef - Deva L, Shah C, Yagnik B, Solanki H, George LB. Principles and Practices of Biomedical Waste Management: A Case Study of Selected Hospitals of Ahmedabad City.
2019. https://www.researchgate.net/publication/333893125_Principles_and_Practices_of_Biomedical_Waste_Management_A_Case_Study_of_Selected_Hospitals_of_Ahmedabad_City - Messner W. The institutional and cultural context of cross-national variation in COVID-19 outbreaks. medRxiv. 2020. doi:10.1101/2020.03.30.20047589
CrossRef - Arcot PJ, Kumar K, Mukhopadhyay T, Subramanian A. Potential challenges faced by blood bank services during COVID-19 pandemic and their mitigative measures: The Indian scenario. Transfus Apher Sci. 2020;59(5):102877. doi:10.1016/j.transci.2020.102877
CrossRef - Kumar V, Singh SB, Singh S. COVID-19: Environment concern and impact of Indian medicinal system. J Environ Chem Eng. 2020;8(5):104144. doi:10.1016/j.jece.2020.104144
CrossRef - Ministry of Environment, Forests and Climate Change, Government of India. Bio-Medical Waste Management Rules-2016. New Delhi. 2016. http://www.indiaenvironmentportal.org.in/files/file/BWM%20Rules.%202016.pdf
- Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi:10.1016/j.jaut.2020.102433
CrossRef - Sharma HB, Vanapalli KR, Cheela VS, et al. Challenges, opportunities, and innovations for effective solid waste management during and post COVID-19 pandemic. Resour Conserv Recycl. 2020;162:105052. doi:10.1016/j.resconrec.2020.105052
CrossRef - Hossain I, Mullick A, Bari S, Islam M. Pandemic COVID-19 and Biomedical Waste Handling: A Review Study. 2020. https://www.researchgate.net/publication/ 341763507_Pandemic_ COVID-19_and_Biomedical_Waste_Handling_A_Review_Study
CrossRef - Chitra J, Rajendran SM, Mercy JJ, Jeyakanthan J. Impact of COVID-19 lockdown in Tamil Nadu: Benefits and challenges on environment perspective. IJBB Vol574 August 2020. 2020. https://www.researchgate.net/publication/350224476_Impact_of_covid-19_lockdown_in_tamil_nadu_Benefits_and_challenges_on_environment_perspective
- Mossa-Basha M, Medverd J, Linnau KF, et al. Policies and Guidelines for COVID-19 Preparedness: Experiences from the University of Washington. Radiology. 2020;296(2):E26-E31. doi:10.1148/radiol.2020201326
CrossRef - World Health Organization. Rational use of Personal Protective Equipment (PPE) for coronavirus Disease (COVID-19). Interim Guidance. 2020. https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nC0V-IPCPPE_use-2020.2-eng.pdf.s
CrossRef - Mysore V, Savitha AS, Venkataram A, et al. Recommendations for Cutaneous and Aesthetic Surgeries during COVID-19 Pandemic. J Cutan Aesthet Surg. 2020;13(2):77-94. doi:10.4103/JCAS.JCAS_83_20
- Singh P. Biomedical hazard: Untended challenge of pandemic- COVID-19. 2020. https://www.nationalheraldindia.com/health/biomedical-hazard-untended-challenge-of-pandemic-covid-19
- Anderson RM, Heesterbeek H, Klinkernberg D, Hollingsworth TD. How will country based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931-934. doi:10.1016/S0140-6736(20)30567-5
CrossRef - Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. The Lancet Respiratory Medicine. 2020;0(0). doi:https://doi.org/10.1016/S2213-2600(20)30076-X
CrossRef







